I just saw dr Anne Peters talking on Medscape why the Look AHEAD trial was stopped:
http://www.medscape.com/viewarticle/772429?src=mp&spon=38
As a reminder, the trial failed to show over a period of 11 years that modest weight loss and exercise can decrease CV events and death in patients with type 2 DM. There were some benefits however, like less OSA and urinary incontinence, slower decline in mobility in overweight adults. Further analysis of data from the trial are still underway. In general there were few CV events in both groups.
It seems like another thing taken for granted in medicine is not that clear-cut when tested under the scrutiny of a RCT or is it? What is important to note, patients in the control group did not gain weight and actually lost some weight (1%), also in general the groups were fairly well-controlled in terms of their diabetes (A1c 7.3%) and lipids (LDL 112 mg/dL) comparing to a significant number of patients we see. Should the population studied be different? If somebody starts with an A1c of 7.3% and with weight loss and exercise is able to get it down to lets say 6.9%, do we think it make a difference in her CV outcomes.
What also is noticeable is the amount of weight loss the intervention group was able to achieve with this considerable amount of help - 8.6% in the first year, which was not sustained and stayed at about 5% for the rest of the study. Losing weight is very hard!
Tuesday, October 23, 2012
Monday, February 13, 2012
Does this patient have a chronic wound infection?
Another article from JAMA series of articles on the rational clinical examination:
JAMA, February 8, 2012 - vol. 307, No. 6
The only proven indicator on history was INCREASING PAIN, however lack of it did not rule out infection.
Other symptoms and signs, which are commonly used, were not helpful in making the diagnosis, i.e.
- Erythema
- Edema
- Heat
- Foul odor
- Discolored granulation tissue
- Serous exudate
- Purulent exudate
- Sanguinous exudate
- Delayed healing
- Wound breakdown
- Pocketing
What is interesting, when IDSA criteria for diagnosing infected diabetic foot ulcers were studied, they were found to lack utility (Se and Sp 50%), which turned out to be both surprising and dissapointing, it highlights the difficulty of making the diagnosis.
Non-invasive test that appeared promising - quantitive swab culture with Levine technique - swab is rotated an area of 1x1 cm for 5 seconds with sufficient pressure to extract fluid from within the wound tissue. Positive test made infection more likely, negative test made it less likely.
JAMA, February 8, 2012 - vol. 307, No. 6
The only proven indicator on history was INCREASING PAIN, however lack of it did not rule out infection.
Other symptoms and signs, which are commonly used, were not helpful in making the diagnosis, i.e.
- Erythema
- Edema
- Heat
- Foul odor
- Discolored granulation tissue
- Serous exudate
- Purulent exudate
- Sanguinous exudate
- Delayed healing
- Wound breakdown
- Pocketing
Classic signs of wound infection, evaluated in isolation from the clinical context and other findings, are not particularly helpful in diagnosing infection in a chronic wound (LR 0.8-2.3). Available studies suggest that the character of wound fluid exudates is most likely not useful as predictor of infection when the reference standard is a deep tissue biopsy culture.
What is interesting, when IDSA criteria for diagnosing infected diabetic foot ulcers were studied, they were found to lack utility (Se and Sp 50%), which turned out to be both surprising and dissapointing, it highlights the difficulty of making the diagnosis.
Non-invasive test that appeared promising - quantitive swab culture with Levine technique - swab is rotated an area of 1x1 cm for 5 seconds with sufficient pressure to extract fluid from within the wound tissue. Positive test made infection more likely, negative test made it less likely.
Saturday, February 11, 2012
Get up and go
Screening test for fall risk in the elderly.
Should be performed in around 10 seconds if you ask the patient to walk 3 meters.
Nice chart to document results.
Should be performed in around 10 seconds if you ask the patient to walk 3 meters.
Nice chart to document results.
Friday, January 27, 2012
Iron (1) - Physiology
NEJM January 26, 2011 - two articles on iron pathophysiology, one on iron overload the other on minihepcidins. It motivated me to review iron physiology.
How much iron do we have? ~4 grams
Absorption in duodenum 1-2mg/day, transport by transferrin, utilization by BM and muscle, storage as ferritin in liver and reticuloendothelial cells (ferritin can be oxidized to hemosiderin), loss mainly by sloughed mucosal cells.
Iron store regulation is achieved by regulating iron absorption, there are no physiological means of iron excretion!
Iron absorption:
Bioavailability: heme > Fe 2+ > Fe 3+
Why heme is better absorbed? Different mechanism.
What form of iron is absorbed?
Iron is rapidly oxidized in physiologic pH, low pH slows this process.
Most dietary iron is turned into it's ferric form (Fe 3+), which is insoluble. Ferric iron is reduced by an enteral brush border enzyme to ferrous (Fe 2+) so the DMT-1 can transport it into the cell. Low gastric pH and vitamin C facilitate this process by slowing iron oxidation.
Where? Duodenal enterocytes
How? DMT-1 which stands for divalent metal transporter-1, so a lot of divalent metal get in this way and can compete with iron. Examples? Lead, copper,
cobalt, zinc, strontium, cadmium
What next? Iron stays in the cell as ferritin or gets out transfered by ferroportin
What helps ferroportin?
Hephaestin, a copper-dependent enzyme, oxidizes iron back into ferric form to help iron efflux from the cell; it is found mainly in the intestinal villi;
Two key proteins in iron physiology:
1. Ferroportin - transporter, which transports iron out of cells;
2. Hepcidin - liver peptide, binds to ferroportin stimulating its internalization and lysosome degradation
How do we lose iron? Sloughing of enterocytes. How does iron know to get into enterocytes to be lost?
High hepcidin -> low ferroportin -> iron stays in entrocytes -> epithelium sloughed -> iron loss
So iron never gets out of the enterocytes in the first place!
Iron transport
Why iron cannot be free? It's dangerous! Free radical production by the Fenton's reaction.
Iron physiology:
How much iron do we have? ~4 grams
Absorption in duodenum 1-2mg/day, transport by transferrin, utilization by BM and muscle, storage as ferritin in liver and reticuloendothelial cells (ferritin can be oxidized to hemosiderin), loss mainly by sloughed mucosal cells.
Iron store regulation is achieved by regulating iron absorption, there are no physiological means of iron excretion!
Iron absorption:
Bioavailability: heme > Fe 2+ > Fe 3+
Why heme is better absorbed? Different mechanism.
What form of iron is absorbed?
Iron is rapidly oxidized in physiologic pH, low pH slows this process.
Most dietary iron is turned into it's ferric form (Fe 3+), which is insoluble. Ferric iron is reduced by an enteral brush border enzyme to ferrous (Fe 2+) so the DMT-1 can transport it into the cell. Low gastric pH and vitamin C facilitate this process by slowing iron oxidation.
Where? Duodenal enterocytes
How? DMT-1 which stands for divalent metal transporter-1, so a lot of divalent metal get in this way and can compete with iron. Examples? Lead, copper,
cobalt, zinc, strontium, cadmium
What next? Iron stays in the cell as ferritin or gets out transfered by ferroportin
What helps ferroportin?
Hephaestin, a copper-dependent enzyme, oxidizes iron back into ferric form to help iron efflux from the cell; it is found mainly in the intestinal villi;
Two key proteins in iron physiology:
1. Ferroportin - transporter, which transports iron out of cells;
2. Hepcidin - liver peptide, binds to ferroportin stimulating its internalization and lysosome degradation
High hepcidin -> low ferroportin -> iron stays in entrocytes -> epithelium sloughed -> iron loss
So iron never gets out of the enterocytes in the first place!
Iron transport
Why iron cannot be free? It's dangerous! Free radical production by the Fenton's reaction.
Fe2+ + H2O2 ----> Fe3+ + .OH + OH-
Fe3+ + H2O2 ----> Fe2+ + .OOH + H+
It is bound to transferrin.
Utilization
1. BM -> erythroid precursors -> hemoglobin
2. Muscle -> myoglobin
Storage
1. Liver -> hepatocytes and Kupffer cells (reticuloendothelial cells)
2. Reticuloendothelial system
So where in our bodies is most of the iron contained?
Tricky question... in circulating RBC's (~1800 mg), almost half.
Sputum in bronchitis
COPD exacerbation is defined by:
- increase in cough
- increase in dyspnea
- change in sputum quality/quantity
 Recent study confirms the correlation between sputum color and the presence of potentially pathogenic bacteria. Especially yellow or green sputum was more predictive than sputum purulence or dyspnea in acute exacerbations.
Recent study confirms the correlation between sputum color and the presence of potentially pathogenic bacteria. Especially yellow or green sputum was more predictive than sputum purulence or dyspnea in acute exacerbations.
Currently when do we use abx?
All three above-mentioned criteria.
When we use two criteria, one has to be change in sputum.
- increase in cough
- increase in dyspnea
- change in sputum quality/quantity
 Recent study confirms the correlation between sputum color and the presence of potentially pathogenic bacteria. Especially yellow or green sputum was more predictive than sputum purulence or dyspnea in acute exacerbations.
Recent study confirms the correlation between sputum color and the presence of potentially pathogenic bacteria. Especially yellow or green sputum was more predictive than sputum purulence or dyspnea in acute exacerbations.Currently when do we use abx?
All three above-mentioned criteria.
When we use two criteria, one has to be change in sputum.
Saturday, January 21, 2012
Metabolic Alkalosis
Great article on the pathophysiology of metabolic alkalosis by F. John Gennari.
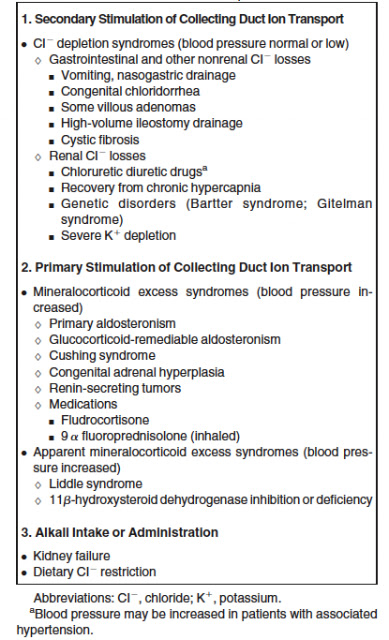
Classification based on pathophysiology:
Pathophysiology of metabolic alkalosis sustainment:
Proposed diagnostic approach:
Classification based on pathophysiology:
Pathophysiology of metabolic alkalosis sustainment:
Proposed diagnostic approach:
The Happy Hospitalist
Blog - great billing workshop
Monday, January 16, 2012
Plantar fasciitis
55 yo school teacher present with several weeks of heel pain...
Most common cause of heel pain -> plantar fasciitis
Pathology is more degenerative than inflammatory so the name should be probably different.
Classic presentation:
- intense, sharp pain with first couple steps in AM
- pain located at the plantar fascia origin (medial tubercle of calcaneus)
- no neurologic symptoms
"windlass test" - passive dorsiflexion of the toes reproduces pain (specific, not sensetive -> negative test tells you nothing)
Hx:
- location of pain
- trauma
- CTD
- exacerbating factors (walking barefoot, flat shoes)
Physical exam
- location of pain (plantar fascia origin)
- anatomical deformities (pes planus, pes cavus, loss of heel fat pad)
- windlass test
- neuro exam for motor and sensory abnl (tarsal tunnel Tinel's test -> do it on the medial side!)
Tx:
- wt loss
- exercise! (stretching fascia and strengthening calf, eg. dynamic stretching rolling a can)
- footwear, arch support, NO heel cups
- physical therapy (if pt needs help w/ exercises)
- pain control (tylenol > nsaids, since no inflammation)
- steroid injection (no good data, similar outcomes)
- surgery (last resort)
Ddx:
1. Plantar fascia rupture (acute, ecchymosis)
2. calcaneal fracture (acute injury, point tenderness, pain w/ simult compression of lateral and medial calcaneal surfaces)
3. calcaneal stress fracture (h/o running etc, point tenderness, pain w/ simult compression..)
4. calcaneal apophysitis (Sever dz) -> adolescents
5. tendinitis (pain with resisted motions)
6. bursitis (retrocalcaneal with swelling and erythema)
7. heel fat pad syndrome (diffuse tenderness of the entire body of calcaneus, fat pad atrophy)
7. nerve entrapment (neuro changes, eg. Tinel test positive)
8. longitudinal arch strain (tenderness over longitudinal arch esp mid or anterior)
9. Paget's dz (can occur in bones of foot usually calcaneus, h/o headaches, hearing loss, bowed tibias, kyphosis)
10. tumor (constant deep bone pain; late constitutional symptoms)
reference: ITC in Annals of Int Med, Jan 3 2012
Most common cause of heel pain -> plantar fasciitis
Pathology is more degenerative than inflammatory so the name should be probably different.
Classic presentation:
- intense, sharp pain with first couple steps in AM
- pain located at the plantar fascia origin (medial tubercle of calcaneus)
- no neurologic symptoms
"windlass test" - passive dorsiflexion of the toes reproduces pain (specific, not sensetive -> negative test tells you nothing)
Hx:
- location of pain
- trauma
- CTD
- exacerbating factors (walking barefoot, flat shoes)
Physical exam
- location of pain (plantar fascia origin)
- anatomical deformities (pes planus, pes cavus, loss of heel fat pad)
- windlass test
- neuro exam for motor and sensory abnl (tarsal tunnel Tinel's test -> do it on the medial side!)
Tx:
- wt loss
- exercise! (stretching fascia and strengthening calf, eg. dynamic stretching rolling a can)
- footwear, arch support, NO heel cups
- physical therapy (if pt needs help w/ exercises)
- pain control (tylenol > nsaids, since no inflammation)
- steroid injection (no good data, similar outcomes)
- surgery (last resort)
Ddx:
1. Plantar fascia rupture (acute, ecchymosis)
2. calcaneal fracture (acute injury, point tenderness, pain w/ simult compression of lateral and medial calcaneal surfaces)
3. calcaneal stress fracture (h/o running etc, point tenderness, pain w/ simult compression..)
4. calcaneal apophysitis (Sever dz) -> adolescents
5. tendinitis (pain with resisted motions)
6. bursitis (retrocalcaneal with swelling and erythema)
7. heel fat pad syndrome (diffuse tenderness of the entire body of calcaneus, fat pad atrophy)
7. nerve entrapment (neuro changes, eg. Tinel test positive)
8. longitudinal arch strain (tenderness over longitudinal arch esp mid or anterior)
9. Paget's dz (can occur in bones of foot usually calcaneus, h/o headaches, hearing loss, bowed tibias, kyphosis)
10. tumor (constant deep bone pain; late constitutional symptoms)
reference: ITC in Annals of Int Med, Jan 3 2012
Friday, January 13, 2012
Meth Mouth
After watching Winter's Bone and hearing Mark's Crislip podcast about a case of Strep discitis in a meth user (he was actually using it iv, not smoking or snorting), I read more about meth use and it's health implications, since my exposure to patients with this problem is limited. Meth appears to be more popular in rural areas rather than inner-city areas, were crack and heroin seem the hard drug of choice.
What I found interesting physical-finding-wise is the prevalence of meth mouth.
Meth mouth = accelerated teeth decay and loss secondary to a combination of factors:
- poor oral hygiene
- xerostomia (dry mouth)
- bruxism (teeth grinding)
- carbonated beverages
Example of meth mouth below:
What I found interesting physical-finding-wise is the prevalence of meth mouth.
Meth mouth = accelerated teeth decay and loss secondary to a combination of factors:
- poor oral hygiene
- xerostomia (dry mouth)
- bruxism (teeth grinding)
- carbonated beverages
Example of meth mouth below:
Vitamins
My wife is pregnant and taking her prenatal vitamins. Obviously folate is the most important one, its role in preventing neural tube defects is well-documented. Today during breakfast she said I could be taking some too as a supplement to my diet, so should I?
Probably not. No good data, that I am aware of, showing benefit of taking vitamin supplements exist. Actually all studies I could recall showed no benefit or potentially harm. That's what I told my wife. What I also knew for sure, is that our morning conversation took place in the wake of a recent publication by Mursu and colleagues of a large observational study showing increased mortality rate in older women taking dietary supplements.
However, I thought I'll spend some more time today googling and pubmeding.
Let's start with the USPSTF. In the 2003 recommendation the USPSTF stated there is insufficient data to recommend for or against the use of supplements with vitamin A, C, or E, multivitamin with folic acid, or antioxidant combinations for cardiovascular disease and cancer prevention. They recommend against the use of beta-carotene.
Publication by Mursu et al. I mentioned above is not the first report showing potential risks of taking supplements. In 2007 a review of randomized trials published in JAMA showed a possible increase in mortality with vitamin A and beta-carotene. Not with selenium or vitamin C however. Beta-carotene was also associated with higher rate of lung, prostate an stomach cancer in the ATBC Cancer Prevention Study.
Another study looking at antioxidant role in CAD when given alone or combined with simvastatin and niacin (HATS study) showed antioxidants attenuate the beneficial effect of these medications on LDL and HDL levels and on clinical end-points. Also a recent Cochrane review showed no benefit of antioxidant supplements in primary or secondary prevention in various diseases.
Seems I will not take the vitamins after all, but even more I will not recommend them to my patients and warn them of potential harms if they are already taking them.
Subscribe to:
Comments (Atom)